Recognition
Pediatric Respiratory Assessment Measure (PRAM) score is used to assess the asthma exacerbation severity. A score of 4-7 classifies as moderate asthma, and 8-12 classifies as severe. For more information on the management of moderate and severe asthma, see sections below.
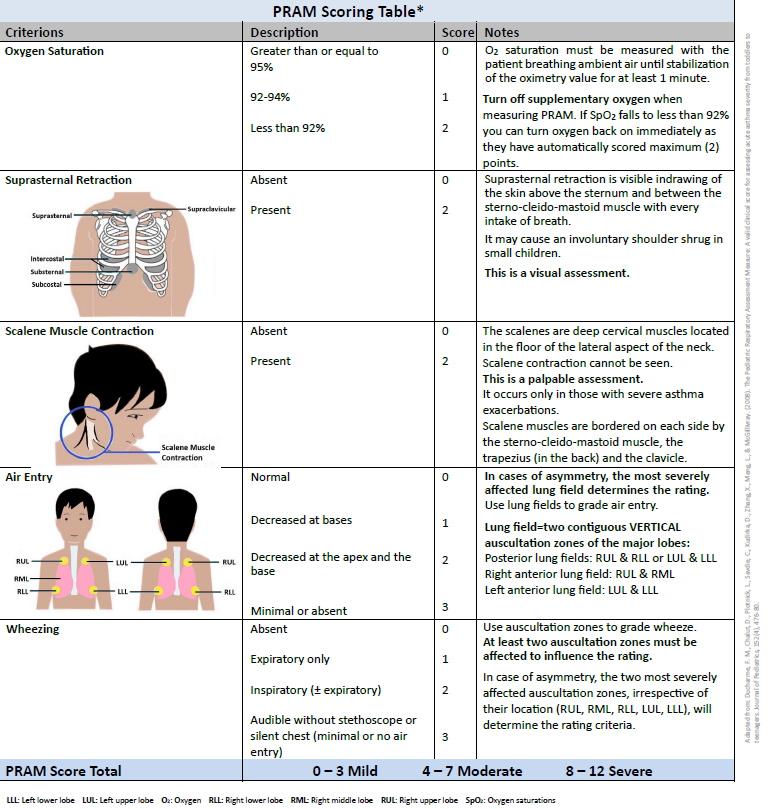
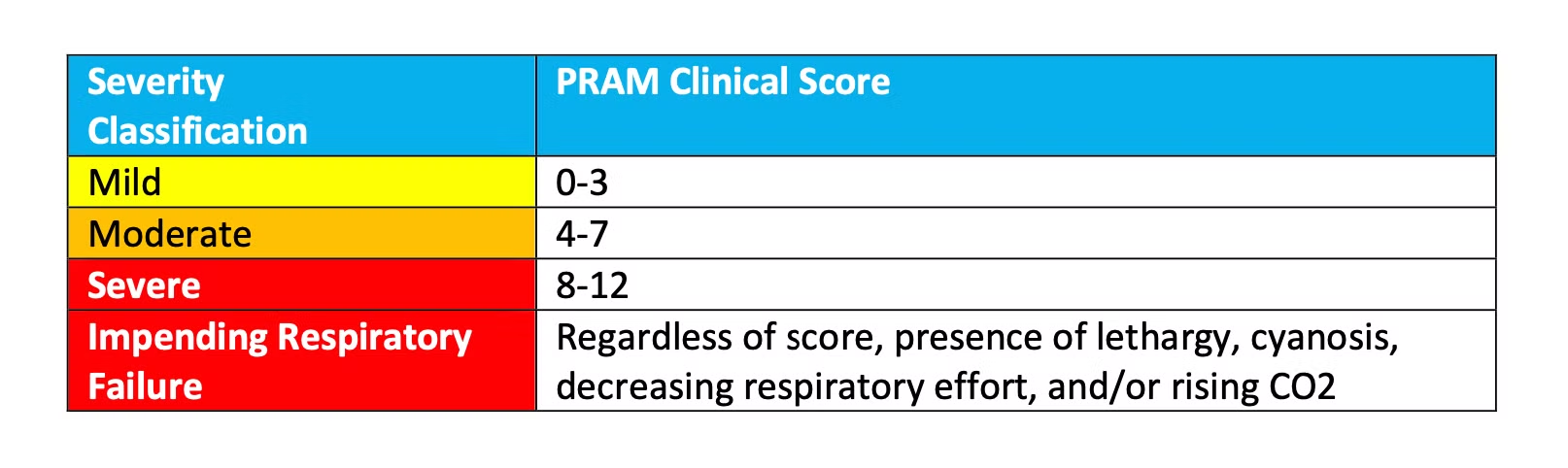
- Caution: Decreased level of consciousness (LOC), lethargy, cyanosis, decreasing respiratory effort and/or rising PCO2 indicates impending respiratory failure
Child Health BC Provincial Asthma Guideline [Internet]. Child Health BC; 2024. Available from: Asthma | CHBC (childhealthbc.ca)
Management – Mild to Moderate (PRAM Score 0-7)
INITIAL MANAGEMENT (MILD TO MODERATE)

Respiratory Support
Provide low flow nasal cannula or facemask supplemental oxygen to maintain SpO2 greater than or equal to 92%.
Medication Administration
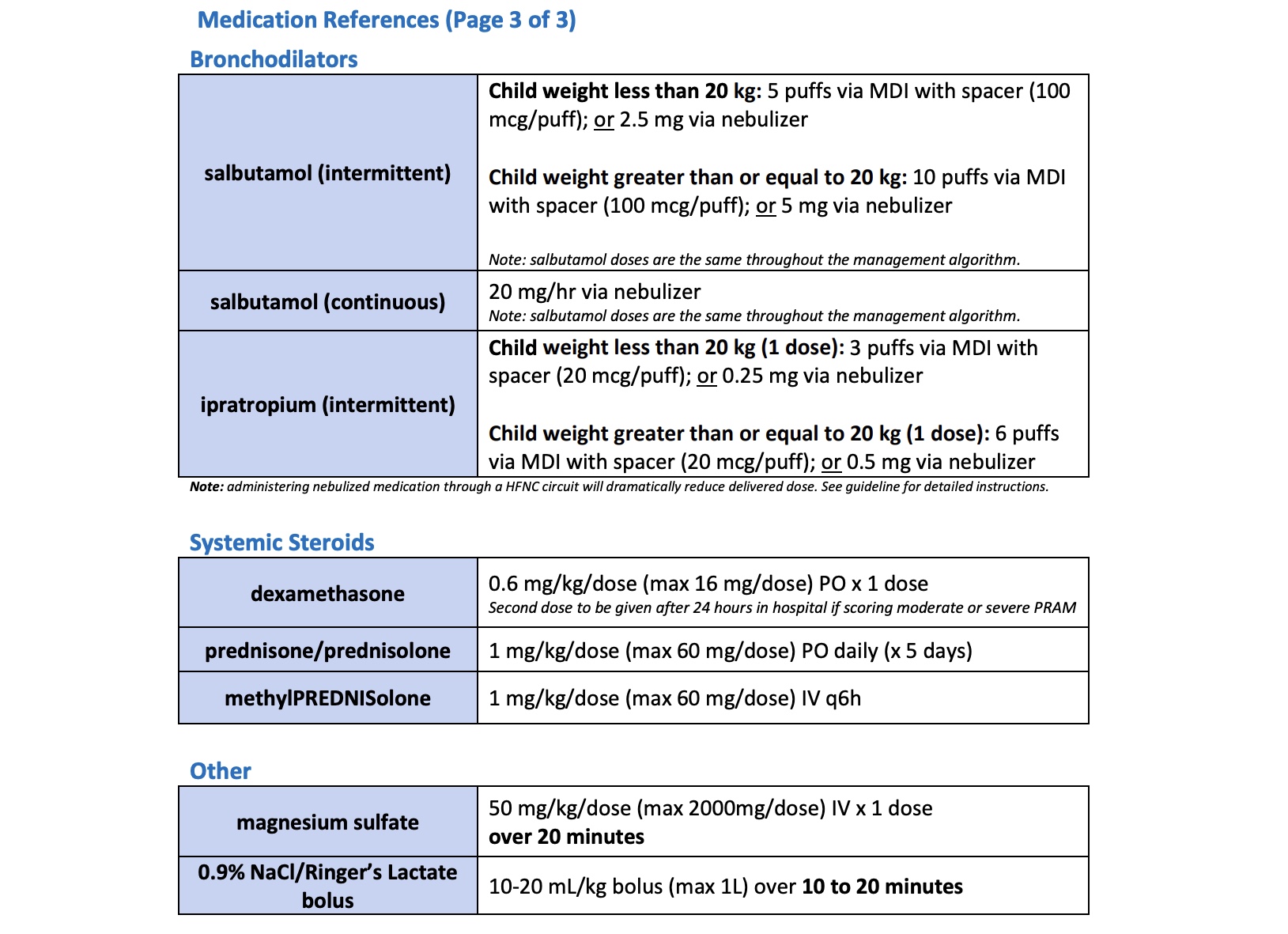
The PRIORITY in management of an asthma exacerbation is the appropriate delivery of bronchodilator therapy and early steroid administration.
Bronchodilator treatment with MDI with spacer and mouthpiece or mask has equivalent deposition with less side effects and decreased length of stay compared to nebulization with a small-volume nebulizer (SVN) for patients with mild to moderate asthma exacerbations. If patient demonstrates competence (usually > 5 years of age), use a spacer with a mouthpiece. For younger children, use a spacer with a mask.
Ongoing Management

Child Health BC Provincial Asthma Guideline [Internet]. Child Health BC; 2024. Available from: Asthma | CHBC (childhealthbc.ca)
Management – Severe (PRAM SCORE 8-12)
Initial Management

Respiratory Support
Only consider the use of HFNC when simple face mask oxygenation is inadequate and BiPAP is not available. It is recommended to consult with the local pediatrician on-call prior to initiating. If no pediatrician is available, call CHARLiE via ZOOM/phone and a higher level of care center via PTN.
Intubation is a high-risk procedure in patients with severe asthma exacerbation due to potential cardiovascular collapse, pneumothorax and ventilation challenges. It must be considered in cases of impending respiratory failure when other therapies have failed and should be performed by the most skilled airway provider available (e.g., anesthetist), ideally in consultation with PICU via PTN. Refer to "Intubation"
Ongoing Management

Medication Administration
In patients with severe exacerbations WHO DO NOT IMPROVE after initial MDI or nebulization treatment, it is recommended to provide continuous nebulization therapy of 60 minutes or more via large volume chamber or vibrating mesh nebulizer (VMN). If not available, a small volume nebulizer with repeated doses given “back-to-back” is an option.
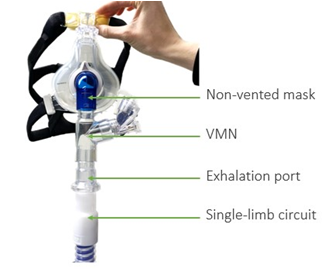
Provide continuous nebulizer therapy utilizing a VMN for patients with:
- Severe exacerbations OR PRAM score of 8 to 12; AND
- On non-invasive ventilation (NIV) or invasive ventilation.
Non-Invasive Ventilation
Dual-Limb Circuits (ie. Hamilton T1 ventilator, Servo-U ventilator, etc.)
- Place the VMN on the dry side of the humidifier pot.
- Use a non-vented patient interface.

Single-Limb Circuits (ie. Trilogy ventilators, Breas Vivo 45LS ventilator, etc.)
- Place the VMN between the patient interface and exhalation port.
- Use a non-vented patient interface.
High Flow Nasal Cannula
If the patient is being treated with HFNC provide the best possible delivery of bronchodilators by following recommendations below whenever possible:
- Pre-oxygenate as needed.
- Remove high flow nasal cannula and deliver medication preferably utilizing an MDI and spacer with mask or mouthpiece; if unable to use MDI, use a small or large volume nebulizer.
For any bronchodilators being delivered by VMN through the high flow circuit:
Reduce the HFNC flow rates to 0.25 L/kg/minute during nebulization of medication while increasing fraction of inspired oxygen (FiO2) to 1 for duration of medication delivery. If patient does not tolerate a reduction in flow, start BiPAP and arrange transfer to higher level of care. If BiPAP is not available at the site, consult with the local pediatrician on-call. If no pediatrician is available, call CHARLiE via ZOOM/phone and a higher level of care center via PTN.
For more information on advanced respiratory support, inhaled medications through advanced respiratory support, and the severe management pathway please refer to the Asthma Edu-Quicks on our website.
Child Health BC Provincial Asthma Guideline [Internet]. Child Health BC; 2024. Available from: Asthma | CHBC (childhealthbc.ca)
Child Health BC. (2025, October). CHBC Asthma Edu-Quick Video Series: 6. Advanced Respiratory Support. [Video]. PHSA Mediasite.
Child Health BC. (2025, October). CHBC Asthma Edu-Quick Video Series: 7. Inhaled Medications Through Advanced Respiratory Support. [Video]. PHSA Mediasite.
Child Health BC. (2025, October). Child Health BC Edu-Quick Series: 3. 2024 Provincial Pediatric Asthma Guideline Severe Management Pathway. [Video]. PHSA Mediasite.
Medication
Child Health BC Provincial Asthma Guideline [Internet]. Child Health BC; 2024. Available from: Asthma | CHBC (childhealthbc.ca)