Provincial Clinical Guideline Framework
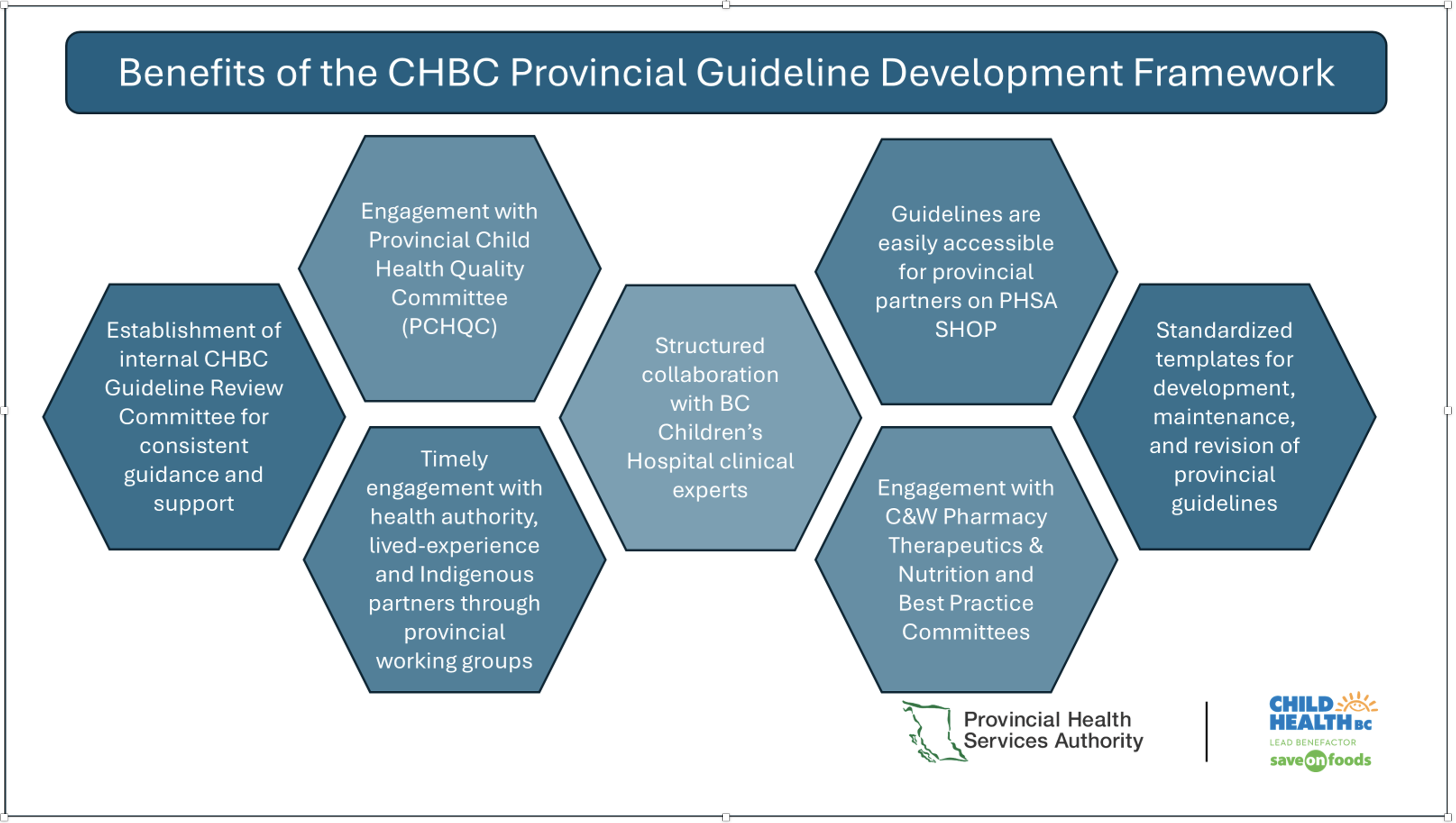
Provincial Pediatric Guidelines are developed utilizing the CHBC Provincial Clinical Guideline Framework. This framework is a multi-stage, quality improvement initiative designed to support the development and revision of provincial clinical guidelines. The framework provides a standardized process, ensuring consistency and meaningful engagement with partners across the province. The framework is supported by approximately 30 templates to guide project teams through each stage of the process.
Current CHBC provincial pediatric guidelines can be found on PHSA SHOP.
Guiding Principles
Anti-racist. CHBC is committed to respecting the experiences of diverse peoples, decreasing inequities (based on race, sexual orientation, gender, ethnicity, religion, age, disability, geography, culture, income, education and sex) and recognizes our obligation to address systemic racism, oppression and discrimination towards all Equity-Deserving Groups.
Gender inclusive language. The terms children, youth, families, and chosen supports are utilized as broadly inclusive terms embracing Two-Spirit peoples, cisgender, transgender, gender non-binary and gender non-conforming.
Child and youth centered care. A philosophy that focuses on listening to young people and providing developmentally appropriate care according to the individual’s understanding of well-being and quality of life. Child and youth centered care emphasizes relationship building focused on trust and respect as well as collaboration between clinician(s) and a child/youth. Care should be individualized and involve a child/youth as active agents in clinical decision making. This includes identifying their family/chosen supports and how they would like them to be involved. It is important to discuss with patients, families and chosen supports, the interprofessional roles and what care can be provided.
Respecting traditional health practices. Under Article 24 of the legal foundational laws of both the United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) and the British Columbia Declaration on the Rights of Indigenous Peoples Act (BC DRIPA), Indigenous patients, families and chosen supports have the right to use traditional medicines and to maintain their health practices. In addition, Article 11 outlines Indigenous legal rights to practice cultural traditions and customs, which includes the right to engage in ceremony at any point in the care trajectory. Indigenous peoples who exercise these rights should be free of discrimination of any kind. Truth and Reconciliation Calls to Action, Article 22, calls upon those in the Canadian healthcare system to recognize the value of Indigenous healing practices and when requested by Indigenous patients, to collaborate with Indigenous healers and Elders to embed them in the treatment provided. Ensure self-identified Indigenous children/youth and their families/chosen supports are made aware of the availability of Indigenous Patient Care Teams (including Patient Navigator/Liaison or similar role) and the supports they provide. When Indigenous Patient Care Teams are not available, contact your health authority/agency Indigenous Health Team or Corporate Indigenous Health. Always receive consent prior to making any referrals. Ensure there is adequate physical space and privacy available for the patient and family/chosen supports to meet with any support service providers.
Family/chosen supports. An approach that recognizes families, including other chosen supports such as trusted advocates, Elders, friends, romantic partners, peers, and other caregivers, in their key role of providing ongoing care and support to a child/youth. This approach is based in a philosophy that service delivery involves a partnership and recognizes that the child/youth’s circle of support impacts their health, wellbeing, safety, and healing.